19year old male with dengue
This is an online E log book to discuss our patients de-identified health data shared after taking his/his guardian signed informed consent . Here we discuss our individual patient's problems through a series of inputs from the available global online community of experts with an aim to solve those clinical problems with collective current best evidence based input
A 19 year old male patient came to the ward with chief complaint of fever from four days .
History of present illness :
Patient was asymptomatic 1week back. Patient started to develop high fever with temperature 102 degrees celsius and chills . Had loss of appetite .
Took 1 paracetamol tablet but conditions recurred .
History of past illness :
No history of diabetes mellitus , hypertension , asthma , epilepsy .
Personal history :
No habit of smoking nor alcohol
No Appetite
Mixed diet .
Bowel movemnets are irregular
Family history :
No significant family history
General examination :
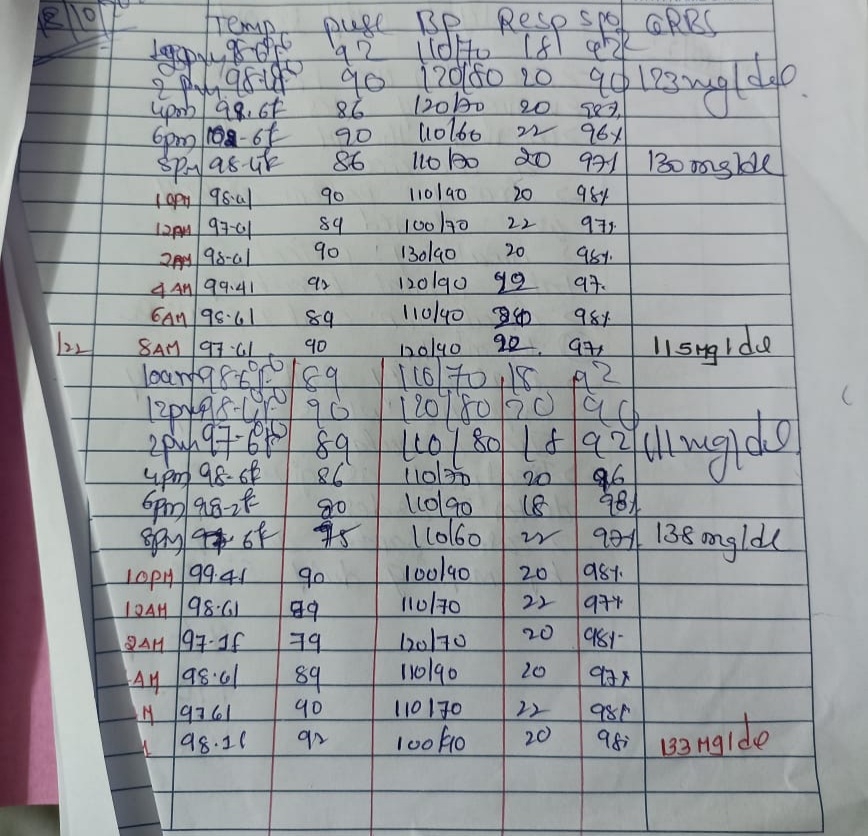
Vitals :
BP : 90/ 50 mmHg
Pulse rate 112/ min
Temp : 103 ° C
RR : 22 per min
Tachycardic
Treatment history :
No specific history.
Systemic examination :
CVS :
S1 S2 heard
Respiration is normal
No skin rashes seen
CNS :
No functional neurological disorders .
Abdomen :
Non tender
Provisional diagnosis :
Dengue
.
Investigations :
Hemogram
Ultrasound report
LFT
ECG
ECG :
Hemogram :
On 18/10/22
Hb : 14.8
TLC : 2,200
Platelet count : 68,000
On 19/10/22
Platelet count : 50, 000
On 20/10/22
TLC : 4,100
Platelet count : 60,000
on 18/10/22
Temp : 98.6 ° F
BP : 110/70
Pulse : 92
On 19/10/22
Temp : 97.6 °F
BP : 120 / 70
Pulse : 79
Intake and output chart
Treatment :